The Impact of Trauma on Child Development, Learning and Behaviour: A Guide for Carers
Children in Care often struggle with more than just the daily challenges of growing up—they're also coping with the long-lasting effects of trauma. As caregivers, it’s essential to understand how trauma can impact a child’s development and learning and how you can support their recovery.
How Trauma Affects Development
Children’s brains are incredibly adaptive, constantly developing new pathways partly based on their experiences. Unfortunately, when those experiences are stressful or traumatic, the brain's survival mechanisms—like the "fight or flight" response—become overdeveloped. This means that traumatised children may adapt to become hyper-vigilant, constantly on edge and quick to react to perceived threats.
There are two broad areas of the brain that we can use to process an event and make a decision. Traumatic childhoods lead to an imbalance between these:
- Primitive Centers (Fight or Flight):
- Healthy role: These parts of the brain are responsible for survival and are fast responses eg the decision to run away from a bear is very quick and you don’t spend a long time balancing all the factors before you decide to do so. You also become less aware of other factors such as pain you may feel in your foot when you are running or what you were meant to be doing when you saw the bear.
- Impact of Trauma: When a child frequently experiences stress or danger, their brain adapts by strengthening the pathways to these primitive centres. As a result, they may become wired to react aggressively or emotionally detach, even in seemingly safe environments.
- Higher Centers (Cognitive & Emotional Functions):
- Healthy role: These areas control more complex thinking and emotional regulation. These thoughts are slower, calm, rational reasoning, balancing different factors out, considering complex factors eg other people's motivations, what were they feeling and what else could be going on.
- Impact of Trauma: Trauma can disrupt the development of these higher functions, leading to fewer neural connections. This can cause delays in speech, social skills and emotional regulation.
This describes how trauma effects:
- Threat - the child is more likely to interpret behaviours as being threatening.
- Reward - the child is not used to having their needs met and the usual reward mechanism encouraging healthy behaviours.
- Memory - the child is more likely to remember negative events and less likely to remember normal every day events.
The Role of Caregivers in Emotional Regulation and Self-Worth
Children begin learning stress management and emotional regulation before they even start school. A nurturing caregiver helps them understand that mistakes are normal and love is unconditional.
However, in cases where correction is excessive or relationships remain unrepaired, children may develop feelings of shame, low self-worth and difficulty managing emotions.
A child's self-image is largely shaped by their caregivers. When caregivers express love, belief in their potential and delight in their presence, children internalise a positive self-concept.
However, trauma can damage this perception, making them feel unworthy and viewing the world as hostile. Their behaviour in school and other environments may further reinforce these negative beliefs if misunderstood.

How Trauma Impacts Learning and Behaviour
For children to learn effectively, they need to feel safe and calm. Traumatised children, however, often remain in a heightened state of alertness, making it difficult for them to focus. Common behaviours include:
- Inability to sit still: Movement helps them manage stress.
- Disruptive behaviour: Acting out can be a coping mechanism for anxiety or shame.
- Aggression: Hyper-vigilance may lead to strong reactions, even to minor stimuli.
- Difficulty with sequencing and planning: Traumatic backgrounds may hinder their ability to predict outcomes, set goals and persist in tasks.

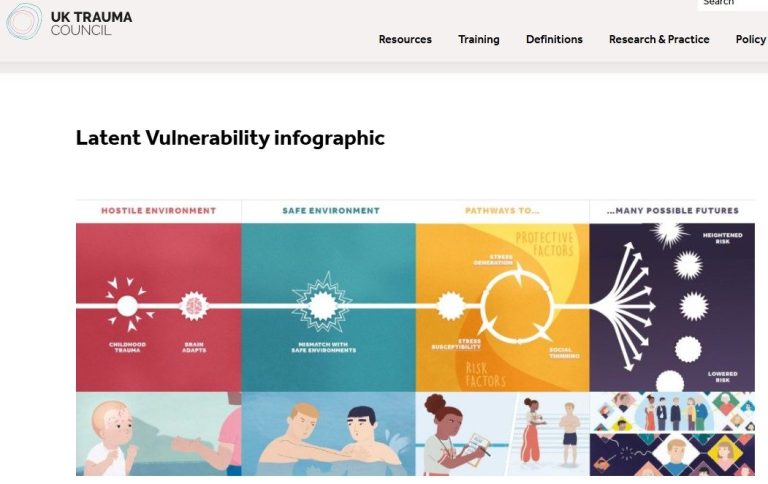
Understanding Latent Vulnerability
Latent vulnerability refers to the hidden risk of future harm due to trauma-related adaptations. These adaptations can increase susceptibility to mental health issues such as anxiety and depression. Factors include:
- Increased stress sensitivity: Feeling overwhelmed easily.
- Stress generation: Experiencing more stressful events due to maladaptive responses.
- Social thinning: Struggling to form and maintain positive relationships.
The good news is that the brain remains adaptable. With the right support, children can recover and develop healthier responses to stress.
A helpful visual resource on latent vulnerability is available here: UK Trauma Council Infographic.
Practical Strategies for Caregivers to Support Recovery
Children in care can recover from trauma and build resilience with the right support.
Key strategies include:
1. Providing Stability and a Safe Environment
A stable environment allows children to regulate emotions and impulses. Positive relationships with caregivers who offer consistent support are essential. Remember that children often test relationships by displaying challenging behaviour. This is not necessarily a sign that a school or placement should be changed but rather an opportunity to strengthen trust and security.
If a caregiver is temporarily unavailable (e.g., on holiday), leaving behind notes or recordings can provide comfort.
2. Using Sensory Techniques
Sensory activities can help regulate emotions.
Techniques include:
Rhythmic movements (rocking, swinging, dancing) to mimic soothing motions from infancy.
Calming stimuli, such as soft music or nightlights, to create a sense of security.
3. Maintaining a Calm Emotional Tone
Demonstrating calm, engaged behaviour teaches children how to manage their emotions. A caregiver's emotional stability provides a model for self-regulation.
4. Encouraging Emotional Awareness
Younger children may benefit from direct conversations about emotions.
Older children may prefer discussing hypothetical situations to explore emotional responses in a less personal way.
5. Showing Empathy
Children in care may have little experience with adults understanding and sharing their feelings. Expressing empathy reassures them that they are valued and that their emotions matter.
6. Fostering a Positive Self-Image
Believing in a child’s potential and reinforcing their strengths is crucial. Encouragement should focus on who they are, not just what they do.
7. Encouraging Stress-Reducing Activities
Hobbies like music, dance and sports can significantly aid recovery and mental well-being. These activities should never be removed as a form of punishment, as they contribute to resilience and self-worth.
For further stress management techniques, see: ACEs Aware: Managing Stress.
Conclusion
Trauma-informed care is about more than managing behaviour—it’s about creating an environment where children in care feel safe, valued and supported. Caregivers play a crucial role in helping children heal by providing stability, empathy and positive reinforcement. By understanding the long-term impact of trauma and responding with compassion, caregivers can make a profound and lasting difference in a child’s life.
Further Information
These are two books that expand on the subjects covered in this blog:
- Parenting Matters: Parenting a child who has experienced trauma https://corambaaf.org.uk/books/parenting-matters-parenting-child-who-has-experienced-trauma
- Parenting Matters: Parenting a child with difficulties in learning caused by trauma https://corambaaf.org.uk/books/parenting-matters-parenting-child-difficulties-learning-caused-trauma
Other useful sources of information:
- UK Trauma Council
- Summary of the effect of trauma on the brain.
- Information on PTSD in Children
- Information specifically on the impact of trauma on unaccompanied asylum seekers.
- Redbridge Safeguarding Children Partnership Multi-Agency Guidance: Trauma informed practice Sept 2024
- IRIIS - a scottish charity looking to improve care provided to people.
- UK Governments definition of Trauma Informed Practice.
- ACES aware - summary about trauma informed practice
- Research into Trauma-Informed Care in Behavioral Health Services.
Thanks for reading this blog post. The content is © copyright to Baker Baker Health. If you find this resource helpful we'd love you to share this webpage freely. If you wish to copy the content or have any comments / suggestions, please email hello@bakerbakerhealth.com and we would be delighted to help!